A Complex Game of Tetris
Originally published by Bev Matthews – 25th July 2018
It’s 7 o’clock on a Friday night as I walk into a dimly lit room full of people sat in front of their respective computers, headsets on, ready for action. They have three or four monitors each and their eyes are darting across them all, swiftly scanning the screens, acknowledging the colour coding and assessing flashing boxes. It looks like some complex game of Tetris!
But this is not a game. It is a 999 ambulance service Emergency Operations Centre (EOC). This one happens to be in the West Midlands, but they exist across England’s 10 NHS ambulance services. The teams in these centres take every 999 ambulance call for their patch 24 hours a day, 7 days a week, 365 days a year. They are trained experts working autonomously but together: responding to calls, following pathways, giving evidenced based advice, allocating crews to emergencies, managing regional resources when a major incident strikes and giving virtually clinical advice to those who need it, when they need it. Everyone is focused on trying to get the best outcome for every patient.
Who are ‘they’?
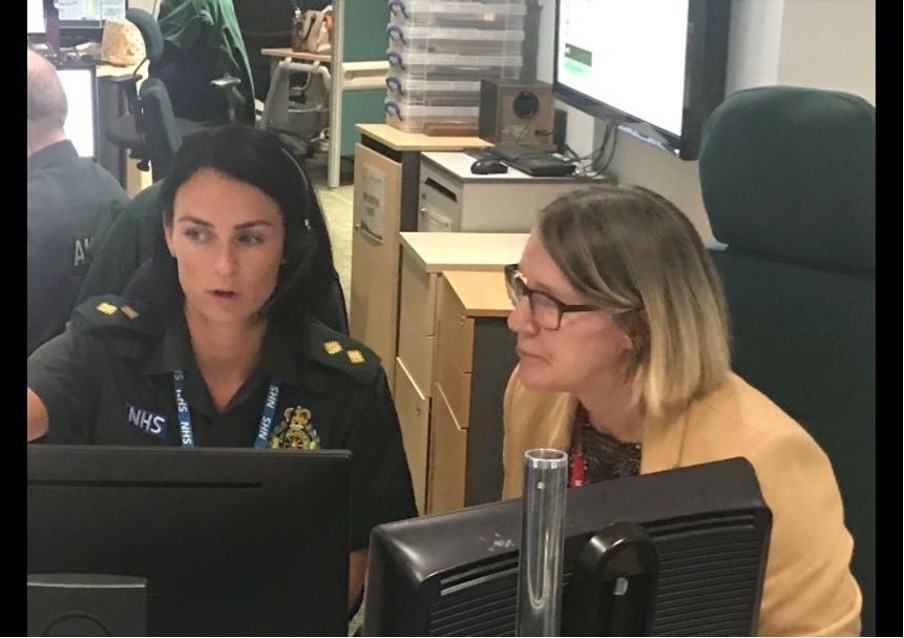
I first met Reena, the EOC Supervisor, at the launch of #ProjectA on the 28th June in London. We were introduced so that I could visit my local service in the West Midlands. I was born in Dudley, trained to be a nurse there (including my return to practice) and now live in a neighbouring town, so it was great to be able to get a better understanding of what they do, and deal with, having also seen for myself the pressures from the local hospital perspective.
I might have thought as I drove there that there would be a hangar at the back full of ambulances and a restroom with paramedics waiting for their next call. I could tell by Reena’s expression that I’m not the first to think this – and I was wrong as it not like that at all. The paramedics and ambulances are stationed at hubs throughout the West Midlands, so that they are able to respond quickly and efficiently to every call, wherever the patient is. Since 2014 paramedics have also been based with nurses in Mental Health Cars, accompanying police officers to incidents where it’s believed people need immediate mental health support.
As I entered the Emergency Operations Centre I was greeted by Jen, the EOC Commander. Jen is a very quietly spoken lady, responsible for the smooth running of the EOC, both today and planning ahead. The teams work in shift patterns of 10 weeks with 12 hour shifts of two days and two nights followed by 18 days fixed annual leave, which all of the staff felt worked for them and gave them an opportunity to organise their holidays, childcare and social events. When I ask how far ahead Jen was now working, she replied “Christmas and New Year”. Why doesn’t the rest of the NHS work like this?
There are protocols and policies in place to ensure a consistent approach across the ambulance trust. Union representatives and staff are involved in putting these together, including looking after the health and wellbeing of the staff. Staff are supported and encouraged to develop and progress into any direction that they wish within the service and are assisted in gaining any relevant qualification that they require if needed. All staff are trained in their respective roles to deal with any major incident or during periods with very high call volumes, always striving to be proactive rather than reactive. For example, during the England football games at the World Cup, Gold Command was put in place, which means senior managers and directors work within the EOC room to support the staff. This helped manage the flow of patients with minimal risk, and also to deal with the management of individual patients where necessary. Duty officers, Controllers and Incident Command Desk staff go through extra training, often via the National Ambulance Resilience Unit, to ensure capability is in place for when it is needed. There is always an EOC manager and an Operational Manager on call 24 hours a day and staff are available for recall to duty if required.
The best way to understand what happens in an environment is for me to experience it for myself. So I shadowed each of the component parts of the EOC, starting at the beginning: when the call comes in. Davina, one of the Call Assessors, has three screens: the first has a map, the middle one had the template for the call details and the third had the log of calls currently in progress. Everyone in the room has this log of all live calls on one of their monitors across the room.
Suddenly there is a buzz in the headset and Davina takes a call. She goes straight into the opening question: “Is the patient breathing?” It’s the local police requesting ambulance assistance at an incident that they are dealing with. Davina is asking contact details, injury queries whilst pathway screens are opening and shifting around the monitors and plans are made. It was all over within about a minute and I just looked at Davina and said: “I have absolutely no idea what happened there!”
The speed with which they work is incredible considering the accuracy and attention to detail that is required – and is key for getting the right response. The details are quickly but accurately recorded, and I can see on the tracker monitor that the job has transferred electronically to the dispatch team and the ambulance is already on its way. It took a few more calls for me to keep up with pace but then the buzzer went off again and this was a very different call. The caller was audibly very distressed and highly anxious. Davina remained calm, with a low tone of voice, and followed the sequence of questions to ensure she quickly could assess the urgency underneath the distress. Within about 30 second (maybe less) the caller was calmer and clearly feeling reassured that he was talking to someone who recognised and respected the need for urgency – a great skill for everyday life too!
The dispatch team is always a set of three: a controller and two dispatchers who are allocating ambulances, assessing capacity and reallocating if necessarily for a crew to be diverted to a Category 1 priority. Gemma and her two dispatchers were covering North Birmingham on Friday night and had a set number of ambulances primarily available to them until 7am Saturday morning. This is a very tactical role and sounded pretty straightforward initially but very quickly the ambulances started to get “stuck” in A&E departments, complexity of patients meant longer times on scene and the crews needed their breaks too – and the 999 calls were still coming through! During the time I was there Gemma, a very skilful technician, also found the time to be compassionate with her colleagues sharing the successful outcome of CPR resuscitation with those involved in the 999 call chain. Then, suddenly, an alert comes in of a stabbing on the site of a local hospital trust. The hospital has had to close their doors temporarily and with immediate effect. One of the dispatchers is making a radio announcement to all paramedics and diverts are initiated for the ambulances on route there to attend other hospitals.
This is an unusual event and so the Regional Control Centre (RCC) now takes on the operational role so that the EOC can continue to respond to 999 calls. The RCC co-ordinates the larger, major and out of the ordinary incidents. The small team in this section were already managing the ambulance service contribution to a chemical incident, working with local trusts where the Emergency Departments were unable to release crews quickly and now also managing the impact from the stabbing. Working in this way means that the incident can be contained in one area of the ambulance service and away from the regular 999 calls. The RCC have access to all of the ambulances across the West Midlands, rather than just one patch, as well as co-ordinating with Helimed and expert advice from trauma paramedics who can liaise with specialised trauma hospitals.
Lastly, but no less important, are the Clinical Support Desks (virtual paramedics to you and me). I met Martin, a highly skilled paramedic, who has over 30 years of experience working on the ambulances. He gives advice to the call assessors if they have a query on what pathway is recommended; paramedics on scene (eg if they need access to the summary care record) and to callers where a virtual consultation will better understand the patient need.
These paramedics also call all of those still awaiting an ambulance response but delayed due to ambulance availability. These calls are an opportunity to review the information collected on the original call, to assess whether there has been a change in the person’s condition, as deterioration might require an escalation of priority, or a decision to self-transport and an improvement in the person’s condition may mean that the ambulance may no longer be required. Access to the patients summary care record and the NHS Directory of Services were invaluable for these virtual clinicians to be able to give the best advice and support, working without the benefit of visual contact with the patient and circumstances around them.
It was really clear to me that the West Midlands Ambulance Service is always looking for new ways of improving patient care, and there was a sense of pride in working there. Staff felt that they would be heard if they put ideas forward for improving the patient experience. Martin, for example has an idea for direct referral of patients to local medical and surgical assessment units. Having worked on such a unit at Russells Hall hospital for my return to practice, I could see how this would work within the safety guidelines that Martin is proposing.
I think we have much to learn from understanding each others’ roles across the system, so do have a look at my #ProjectA idea for improving ambulance services – and add one of your own too!
This was an amazing experience and I am very grateful to West Midlands Ambulance Service NHS Foundation Trust team members for their time, skill and patience. Next weekend I am going to shadow the paramedics in one of the HUBs …
“an emergency call may be the 100th incident of the same nature that day, week or month for the call assessor, but to that member of the public it may be their first emergency and so every call is treated with dignity and respect, even if the issue could have been resolved elsewhere in the health and care system” Jackie, Emergency Operations Centre, Team Leader
