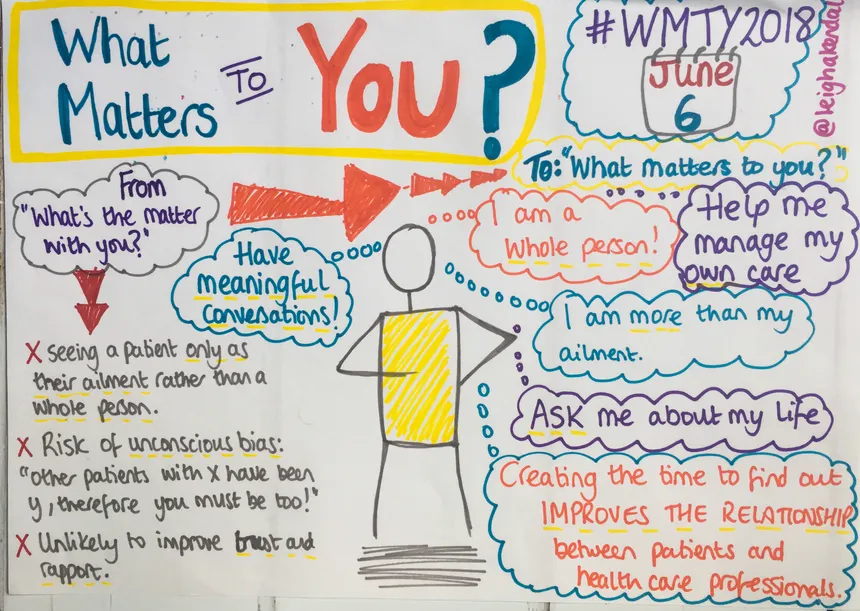
From What’s the Matter with You to What Matters to You
Originally published by Leigh Kendall – 5th June 2018
How many of your conversations are truly meaningful?
A lot of conversations in everyday life are transactional: for example a few words exchanged between you and a member of staff while asking for a coffee in a cafe, being told the price, paying for it. You might exchange a few pleasantries…and hopefully there will be a ‘please’ and a ‘thank you’ in there, too.
Transactional conversations are fine in many contexts – they achieve a goal. Within a healthcare context, though, we need more meaningful conversations, those that shift the focus from “what’s the matter with you?” to “what matters to you?”.
Why is this important?
Evidence shows that taking the time to ask a patient about themselves, to see them as a whole person rather than their ailment helps build a positive relationship between a healthcare professional (or a team of professionals from a range of specialties for those with long-term conditions) and the patient.
Having a meaningful conversation helps build trust and rapport, with the opportunity for the healthcare professional to gain crucial insights about the person’s life, meaning they will be better able to work with the person to find the best way forward for them. This in turn gives the person confidence to manage their condition(s) during their day-to-day life, and to be involved in decisions about their care (it’s often referred to as health activation).
It’s the working with aspect that is crucial here – working together to identify solutions that work for the patient as an individual lead to better outcomes. Those outcomes need to be focused on to the individual, too – and those outcomes can be discovered only by having a meaningful conversations.
The exception may be, of course, emergency life-threatening situations. In other cases, taking the time to ask “what matters to you” is of optimal benefit to the patient and the healthcare professional.
For those living with long-term conditions involving family, friends, and carers in these conversations is also invaluable.

In my own personal experience as a patient, I’ve seen both sides. After my baby son sadly died (I had the rare, life-threatening pregnancy complication HELLP syndrome at 24 weeks) I was diagnosed with post-traumatic stress disorder (PTSD), and spent a lot of time with a range of mental health practitioners. Many of those interactions unfortunately focused on “what’s the matter with you?”. I remember being told that my feelings were a natural response to events (often with quite a dismissive tone) which may well have been true, but what I needed was a way to help me manage those feelings. Those interactions were probably the result of unconscious bias on behalf of the practitioner (“I’ve seen other people with x, therefore you must be the same”.)
When my care was moved to a different practitioner, who took the time to ask what mattered to me, my experience was transformed. PTSD is something that I’ll probably live with for the rest of my life, and as a result of that practitioner’s efforts I am able to live with it.
While meaningful conversations are important in every specialty in health and care every day of the year, there is a particular focus on 6th June, with the international campaign What Matters to You Day. There is a wealth of good practice examples to learn from – if you’re on Twitter, do take the time to look up #wmty18 or #wmty2018 (and if you have good practice examples to share, please do add them so that others can benefit).
I was going to start listing some of the good practice examples – there are so many though, it would make for a very long post! Instead, I thought I’d quote this story that I heard at the International Forum on Quality and Safety in Healthcare during a session on What Matters to You? It’s one of those stories that I’ll never forget, and so succinctly sums up how taking the time to have a meaningful conversation can have a huge impact.
The context is a doctor arriving on a geriatric ward at a hospital in San Francisco. The doctor asks the staff who is their most boring patient? Without hesitation, the staff point to an elderly lady who had been in hospital for a long period of time, had no visitors, and spoke only in monosyllables.
Doctor: “How long have you lived in San Francisco?”
Woman: “Years and years.”
Doctor: “Where did you come from?”
Woman: “Ireland.”
Doctor: “When did you come?”
Woman: “1912.”
Doctor: “Have you ever been in the hospital before?”
Woman: “Once, for a broken arm.”
Doctor: “How did that happen?”
Woman: “A trunk fell on it.”
Doctor: “A trunk? What kind of trunk?”
Woman: “A steamer trunk.”
Doctor: “How did that happen?”
Woman: “The boat lurched.”
Doctor: “The boat? Why?”
Woman: “It hit the iceberg.”
Doctor: “Oh! What was the name of the boat?”
Woman: “The Titanic.”
And so the woman went from being the ‘most boring’ patient to the most interesting.
This type of approach can help you in a number of ways. First and foremost it helps to establish a relationship, but it also helps you to understand the person in the context of their own life and the things that are most important to them. With this crucial insight you are in a much better position to work with the person to find the best way forward for them.
